PATENT DUCTUS ARTERIOSUS (PDA)
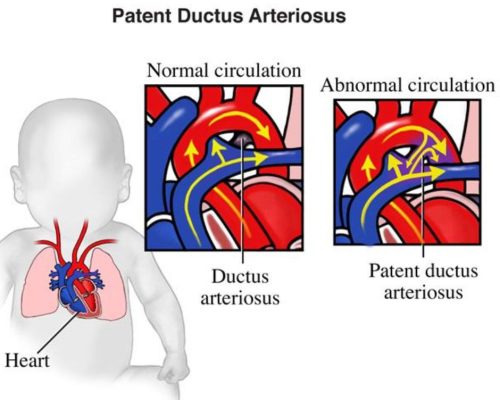
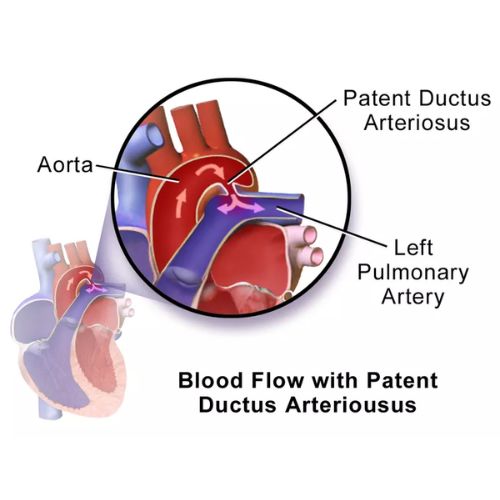
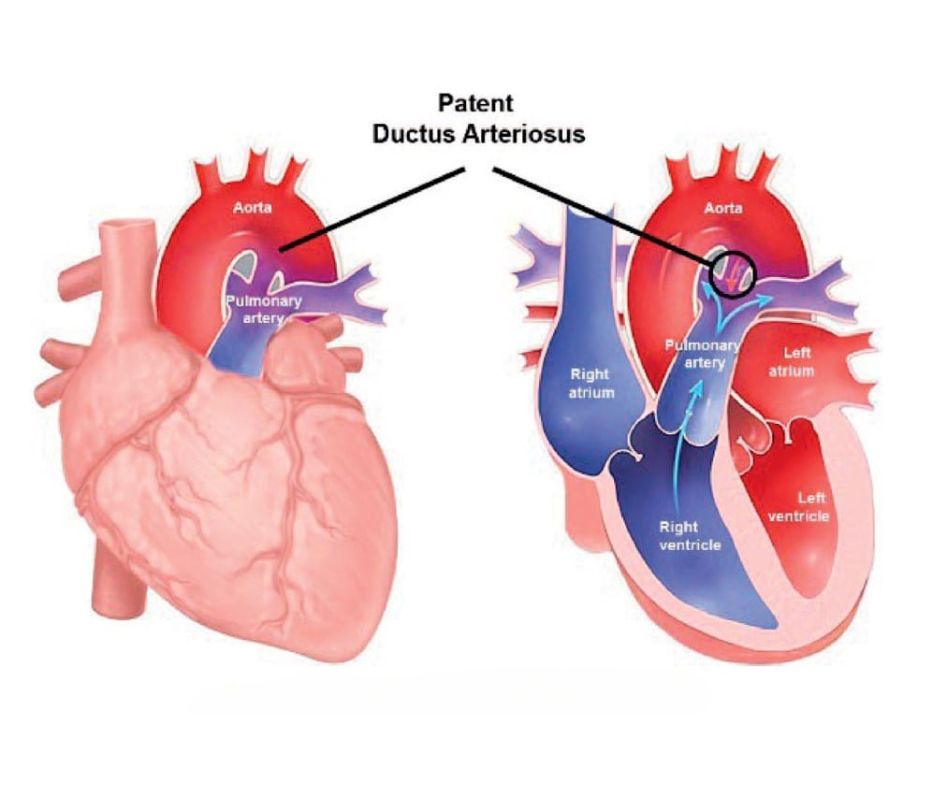
Patent ductus arteriosus, the most common type of extracardiac shunt, represents persistent patency of the vessel that normally connects the pulmonary arterial system and the aorta in a fetus.
Incidence
• PDA occurs in approximately 1 of 2,000 live births, but it is relatively uncommon among the adult population.
• In infants, it accounts for 10% to 12% of all congenital heart disease.
• PDAs are twice as common in female infants as in male infants.
• In rubella syndrome male female are affected equally.
Risk Factors
• Maternal rubella infection
• Birth at high altitude
• Premature birth
• Female sex, and
• Genetic factors
In infants born <28 weeks of gestation, there is a 60% incidence of PDA

EMBRYOLOGY

• The ductus arteriosus is a normal and essential component of cardiovascular development that originates from the distal sixth left aortic arch.
• A PDA is most commonly funnel shaped with the larger aortic end (ampulla) distal to the left subclavian artery, then narrowing toward the pulmonary end, with insertion at the junction of the main and left pulmonary arteries
Fetal Circulation
• The presence of the ductus
arteriosus in the fetal circulation is essential to allow right-to-left shunting of nutrient-rich, oxygenated blood from the placenta to the fetal systemic
circulation, thereby bypassing the fetal pulmonary circuit
• In the fetus, the ductus arteriosus is kept open by
> Low arterial oxygen content and
> Placental prostaglandin E2 (PGE2)

Birth
• Several changes occur at birth to initiate normal functional closure of the ductus arteriosus within the first 15 to 18 hours of life.
• Spontaneous respirations result in increased blood oxygen content.
• Prostaglandin levels decrease because of placental ligation and increased metabolism of prostaglandins within the pulmonary circulation by prostaglandin dehydrogenase.
• Generally, the ductus arteriosus is hemodynamically insignificant within 15 hours and completely closed by 2 to 3 weeks
Symptoms
Severity of symptoms depends on the degree of left-right shunting; and it is determined by the size of the PDA, ductal resistance, cardiac output, as well as the systemic and pulmonary vascular resistances.
• Patients with small PDA are asymptomatic.
• With larger PDAs, symptoms may develop.
• The most common symptom is exercise intolerance followed by dyspnea, peripheral edema, and palpitations.

Signs
• Tachycardia and tachypnea may be present in infants with CHF.
• Bounding peripheral pulses
• Wide pulse pressure
• Hyperactive precordium: With a large shunt
• Systolic thrill: may be present at the upper left sternal border.
• The P2 is usually normal, but its intensity may be accentuated if pulmonary hypertension is present.
• A grade 1 to 4 of 6 continuous ("machinery") murmur is best audible at the left infraclavicular area or upper left sternal border.
• An apical diastolic rumble may be heard when the PDA shunt is large.
• Patients with small ductus do not have the above findings.
• The duration of the diastolic murmur reflects pulmonary artery pressures; elevated pulmonary artery pressures lead to a decreased gradient for left-to-right flow through the PDA during diastole, which results in a shorter diastolic murmur.
• As pulmonary pressure increases, the systolic component of the murmur shortens.
• Right-to-left flow may not generate a systolic murmur.
• Differential cyanosis: If pulmonary vascular obstructive disease develops, a right-to-left ductal shunt results in cyanosis only in the lower half of the body.
Investigation
1. ECG
2. CXR
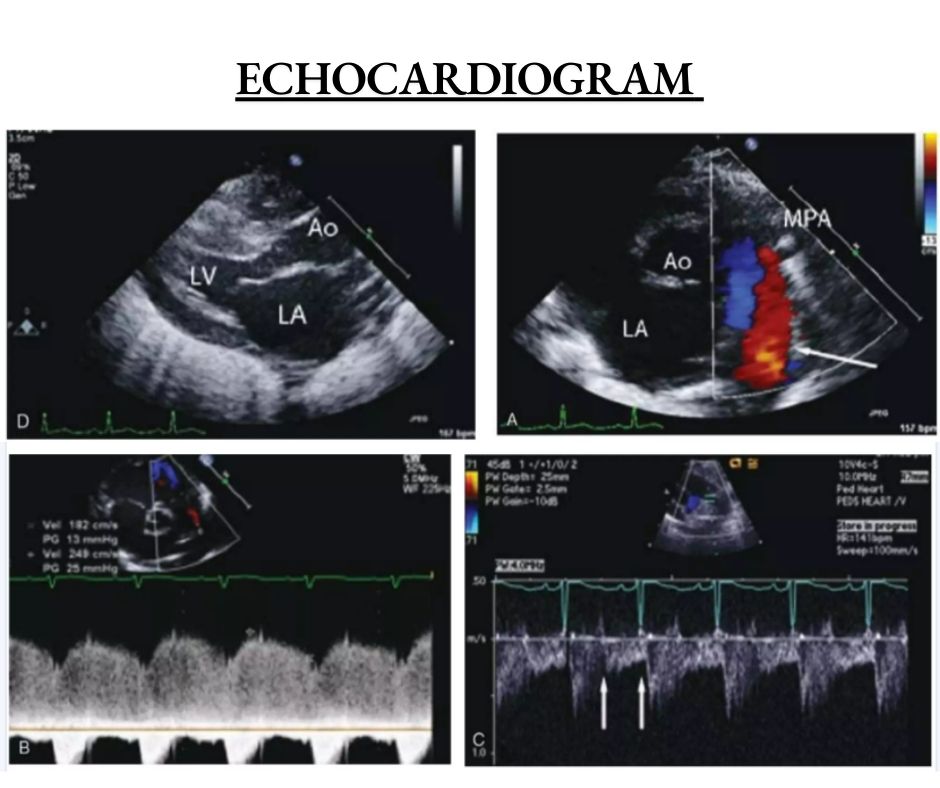
3. ECHOCARDIOGRAM
4. CARDIAC CATHETERIZATION
5. OXYMETRY
6. PRESSURE STUDY
7. LV GRAPHY
8. AORTOGRAPHY
9. MRI
10. CT